
Trusted Exchange Framework and Common Agreement (TEFCA)
On January 19, 2022, the office of the National Coordinator for Health Information Technology (ONC) introduced …
Every year huge amounts of data are created by healthcare organizations in the form of lab results, patient records, and medical images. The federal Health Information Portability and Accountability Act (HIPAA) and State laws require the providers to store this information for years and sometimes even for decades. Therefore, it is necessary that health data archival is a key part of the overall IT plan of an organization.
Through this blog, you will be able to explore:
Data archiving refers to the process of shifting data that are infrequently accessed to repositories with low-cost storage. It forms an important part of an organization’s data management strategy. The basic goals of data archiving include:
In the healthcare industry, a data archiving plan forms an important part of a hospital or health center’s policy or data lifecycle management. It provides a way of retaining information within a reasonable storage budget. The procedure of data archival typically involves automation and supporting tools that help in driving efficiency into the process.
There are a variety of options that health IT leaders can consider for data archiving strategy. These options range from on-site tiered storage within the SAN or Storage Area Network to off-site storage provided by a cloud service provider. Security is one of the key factors that must be taken into consideration, especially in light of the HITECH (Health Information Technology for Economic and Clinical Health) Act’s changes to HIPAA.
Archives of healthcare data are driven typically by EHR/EMR changes, physician retirements, or acquisitions. When a healthcare organization goes through any such transitions, that is where the need to create a healthcare data archive plan steps in. The old legacy systems contain valuable data that is required to be preserved. But again, that comes with the burdens of security and maintenance costs. The best way of maintaining data access that is needed for reference during the process of maintenance elimination and security concerns is by migrating and archiving data.
There is an option of moving a part of the legacy data into the new system during data migration. But simple migration of basic data may not always satisfy the requirements of data retention. The version that is migrated is often not complete and faithful to the original one. Additionally, there are many vendors who would commit to importing a bare data subset and almost always disagree with importing detailed records. To ensure that the data for the ongoing requests for medical records is present when needed, a thorough data archive is highly required.
There are three main steps that are involved in the process of the Healthcare Data Archival. They are as follows:
Step 1: Data extraction - getting the data out of the legacy system The approach for data extraction is dependent on where the data is stored. A proper healthcare data archive partner can help in guiding through various aspects, such as whether the data is in the cloud or hosted locally, whether it is encoded or encrypted or whether there is any data stored in ancillary systems such as ultrasound equipment or EKG machines, which requires extraction. Having a reputable partner for health data archival can help in the selection of the most thorough, cost-effective, and efficient path for data extraction.
Step 2: Data transformation - getting the data in the required form Once the data that is required to migrate or archive is there, it is important that it is converted into a form that would make sense for the use cases of the archive or for fitting into the new system. One of the biggest decisions revolves around whether a static image of each record is required to be created or whether archiving discrete data is required so that there is flexibility in presenting it as and when it would be needed. The complete image that is fixed helps in offering compliance as it is inalterable. While on the other hand, having the archive in the form of discrete data means that the customer reports, which are data-based, could be run if needed.
Step 3: Data storage and access - determining where the data would be stored During the process of creating a data archive, one can choose to house the data in a stand-alone application, use an existing system of document management, or make use of a cloud solution. A few things are, however, needed to be considered while making the data archive storage choices.
While the above steps are necessary in order to successfully archive health data, there are some practices that would ensure that it is done in the best way. Some of the best practices for efficient healthcare data archival are as follows: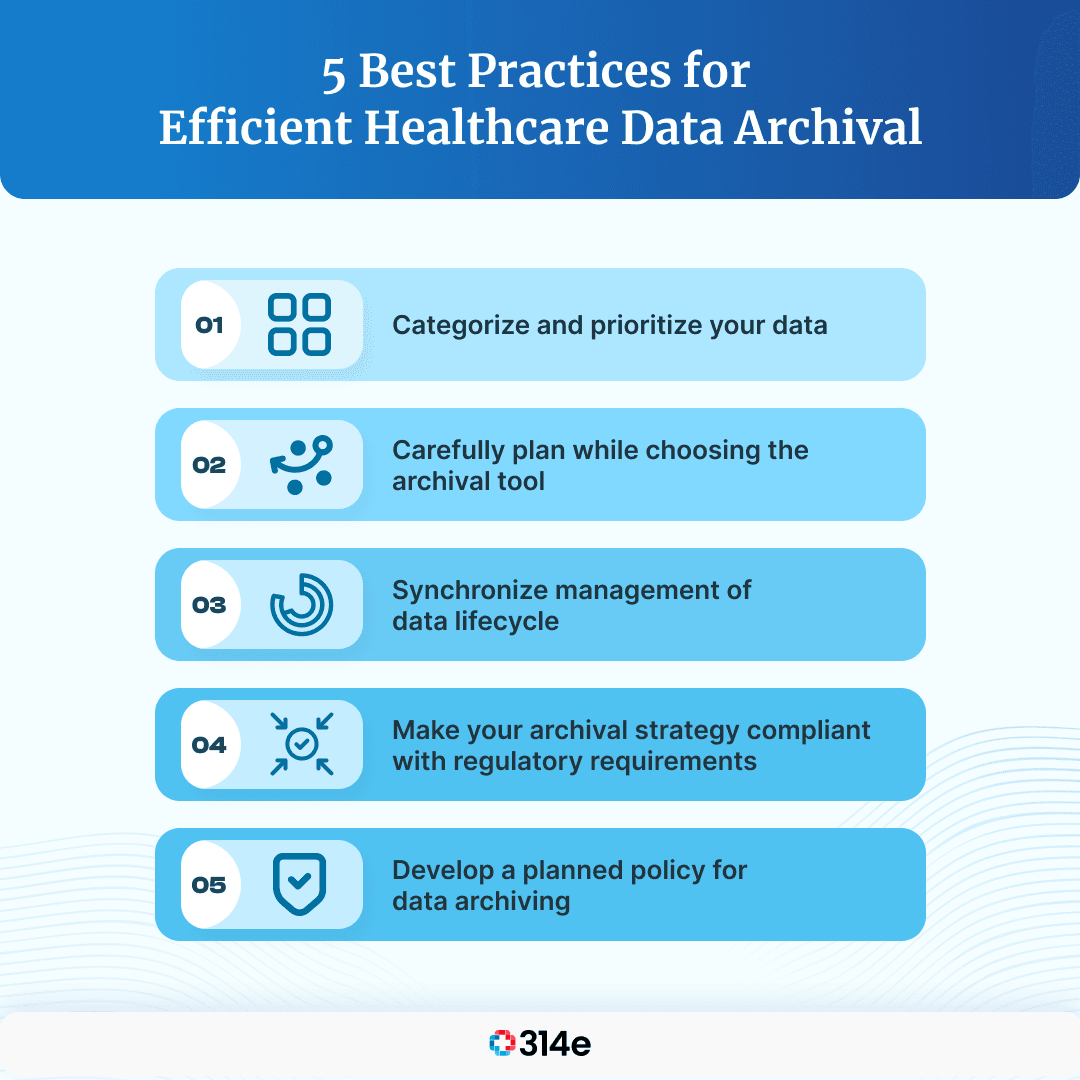
1. Sorting and identifying the data before archiving: This involves checking out the data to be archived and creating an inventory. Categorizing the data into types, prioritizing it, and then carefully considering which data would be required for the ongoing operations and which could be moved for archival purposes are all involved in this process.
2. Synchronizing data archival and management of data lifecycle: Data archive impacts the data lifecycle. While creating the archival plan, considering the lifecycle of the archived data is a good practice.
3. Regulatory compliance planning: This involves making sure that the archive strategy is entirely compliant with compliance regulations that are relevant. If it is needed to enforce strict standards of compliance on behalf of the archival data, but the other archival data could be stored easily, then it might be better to consider creating two separate archives.
4. Selecting the right archival tool: There are various solution types that can help in supporting the data archiving strategy. While some of the tools are devoted to data archiving, others offer end-to-end data solutions with built-in capabilities of archiving.
5. Developing a policy for data archiving: Once all the requirements are assessed for archival data strategy, one can create a comprehensive policy of data archival, which would document all the relevant processes clearly.
Rationalization refers to a strategic initiative, usually denoting that an organization is being reorganized to increase operational efficiency. When it is applied to application portfolios, rationalization aims at explicitly improving efficiency levels through the reduction of complexity and lowering the total cost of ownership.
Rationalization entails the following:
1. Retiring the aging and low-value applications
2. Modernizing the aging and high-value applications
3. Eliminating applications that are redundant
4. Standardizing platforms of common technology and versions
5. Consolidating the applications logically and physically
In the healthcare IT environment, the process of rationalization needs ‘application decommissioning’. This is nothing but a strategic approach that systematically retires costly and outdated legacy applications without compromising compliance requirements or business needs.
To reduce complexity and operational spending, the application portfolio could be rationalized through a set of risk reduction activities, count and application costs. They are:
1. Reducing costs: Eliminating the development, support, infrastructure, and licensing costs of applications of legacy
2. Retiring technical debt: Migrating from platforms that are on-premise for taking a cloud-first approach, removing versions of support software, patterns of legacy architecture, and legacy hardware
3. Eliminating functional redundancy: Removing fragmentation, superfluous integration, and functional overlap
4. Reducing risk: Focusing on and acting to enhance high security, availability, and compliance
Aging technology applications that have significantly outlived support are more vulnerable to threats of cybersecurity significantly. This is not a surprise since there are many legacy systems that are forgotten and hence do not receive any of the latest patches, updates, and remedies of anti-virus to ensure security. Moreover, legacy systems do not typically have active users who could identify abnormal behavior.
All healthcare organizations must formulate their application portfolio risk profile and then rank those applications in terms of their functionality, the type of processed information, and the business value it provides. A comprehensive assessment of risk would make it possible to create a cost-effective and prudent blueprint for remediation, consolidation, and elimination of legacy applications.
Fast Healthcare Interoperability Resources or FHIR® refers to a standard that was published by Health Level Seven International (HL7) for the purpose of electronically exchanging health information. The EHRs or Electronic Health Records of members and patients must be discoverable, available, and understandable as members and patients move around the healthcare ecosystem.
To further support other machine-based processes and automated clinical decisions, the data must be standardized and structured. FHIR® is particularly important for data archival because it aims to simplify implementation without sacrificing the integrity of information. It helps in leveraging theoretical and logical models for providing an easy-to-implement, consistent and rigorous mechanism to exchange data between applications of healthcare.
The modular set of components is built from FHIR® solutions called ‘resources’. These resources could be easily assembled into working systems that help in solving real-world administrative and clinical problems at a fraction price of existing alternatives. Apart from the above-mentioned reasons, there are several other causes why implementing FHIR® could turn out to be extremely beneficial. They are as follows:
1. It could be easily implemented
2. It has a lower bar for developers’ entry
3. It is free to use
4. It is flexible
5. It leverages and co-exists the previous standards that came before
6. It also has a strong web standards foundation
There are a few things that are important to keep in mind while archiving healthcare data. They are as follows:
1. Preserving the complete record integrity: The healthcare organization should be able to preserve the original record with completeness and integrity. It should also have the ability to recreate a record copy in the same way that it existed.
2. Retaining audit trails: This involves ensuring a robust trial of audit is archived and retained for the purpose of capturing precise event sequences. This would help in providing evidence that would explain or justify the actions that have occurred. It is also vital for satisfying e-discovery requests.
3. Avoiding the practice of overlooking version history: Individual clinical items’ version history is a set of major data that is often overlooked during data archiving. This is a practice that should be avoided while archiving healthcare data.
4. The legal risks involved with purging archived data: The ambiguity that is involved with retention guidelines at the federal and state levels while purging archived data results in organizations putting themselves at a considerable amount of legal risk. This involved risks must be taken into account during procedures of healthcare data archival.
Another important thing to note is that data archiving and data backup are not the same thing. While backups intend to restore an existing system in a business continuity or disaster recovery scenario, the strategies of data archiving assume that the system that is in question is no longer there or does not need to exist.
Even though data archiving could be a complex topic to understand, the benefits that it offers make every healthcare organization embrace it as a standard practice. The key strategy to navigating the process of data archival is choosing the vendor who has the right mix of the core capabilities, relevant technologies, and experience to not just successfully complete individual projects of archiving with good customer service but also to help the healthcare IT organizations in doing their part of ensuring the success of initiatives in terms of timeliness, quality and costs.
Join over 3,200 subscribers and keep up-to-date with the latest innovations & best practices in Healthcare IT.

On January 19, 2022, the office of the National Coordinator for Health Information Technology (ONC) introduced …

According to Gartner, 83% of data migration projects either fail or exceed their budgets and schedules. This …

As organizations adopt EHR and mature in data digitization, the reporting needs and complexity grow …